No Products in the Cart
Diabetes, also known as diabetes mellitus, is a chronic disease that affects how your body processes blood sugar. It occurs when your body either doesn't produce enough insulin, or is unable to use insulin effectively.
Insulin is a hormone produced by the pancreas that helps regulate glucose levels in the blood. Without insulin, glucose builds up in the bloodstream, leading to high blood sugar levels.
Diabetes is a serious medical condition that can have a significant impact on the lives of those affected.
Fortunately, improving gut health may be an effective way to control the symptoms associated with diabetes. Recent research has suggested that a healthier gut can help regulate blood glucose levels and, ultimately, lead to improved diabetes management (Kocsis et al., 2020).
Diabetes mellitus comes in two basic types: Type 1 and Type 2.
When you have Type 1 diabetes, your body is unable to produce the hormone insulin, causing your blood sugar to become too high.
Although it can happen at any age, it is frequently diagnosed in children. If your father, mother, brother, or sister has Type 1 diabetes, your risk of getting it is higher as well.
The primary form of treatment for the condition is insulin administration.
The most prevalent type of diabetes is Type 2, accounting for up to 95% of all cases.
It results from either your body not producing enough insulin or the insulin that is generated not functioning effectively (often known as insulin resistance).
Healthy nutrition and more exercise are part of the treatment. Some patients with diabetes Type 2 may be given metformin or insulin as a prescription.
Some of the symptoms of Type 2 diabetes include frequent weeing (polyuria), especially at night, frequent thirst (polydipsia), fatigue (feeling tired), unintentional loss of weight, genital itching, healing difficulties of cuts, and blurred vision.
Everyone is at risk of developing Type 2 diabetes because it is largely influenced by lifestyle.
Even though there is no cure for diabetes, some people can manage it by leading healthy lives.
According to the (Diabetes UK), 4.3 million individuals in the UK (8% of the population) have diabetes; 40 000 children have the disease, and more than 3000 more children are diagnosed each year. Moreover, roughly one million people in the UK have Type 2 diabetes but are undiagnosed (Whicher et al., 2020).
According to reports, over 500 individuals with diabetes die prematurely in the UK each week, the National Health Service (NHS) spends £19 000 on treating diabetes every minute or at least £10 billion every year (10% of the NHS annual budget) (Diabetes UK). Every hour, a person with diabetes requires an amputation (Hex et al., 2012).
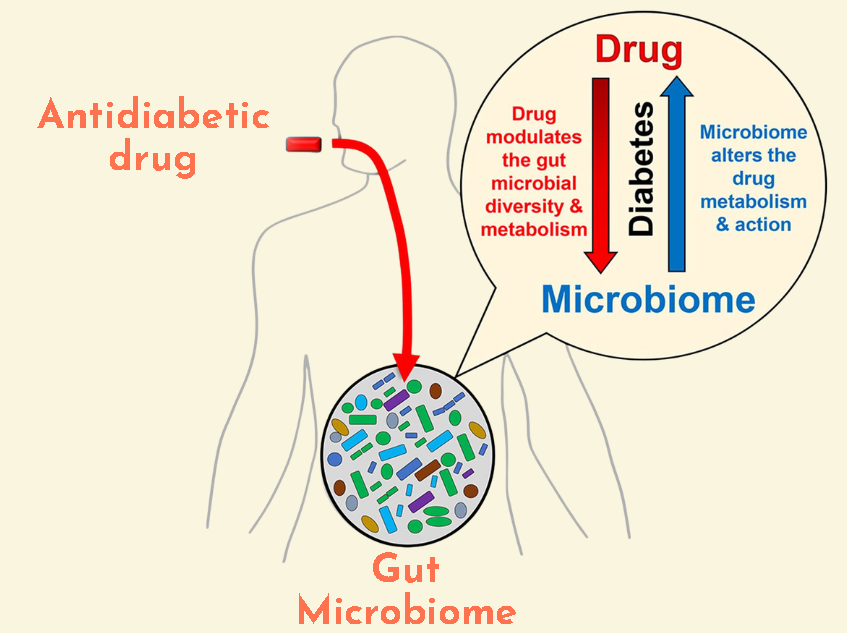
The first drug of choice for treating T2D patients is metformin because it is effective in reducing hyperglycemia without causing adverse effects like hypoglycemia, weight gain, or any cardiovascular complications (Cefalu et al., 2014).
Metabolic function and the gut microbiota are both aided by metformin (Sharma & Tripathi, 2019).
Metformin has been reported to induce mucin expression and decrease tissue inflammation in diet-induced conditions like obesity (Hur & Lee, 2015).
Before delving into the connection between gut health and diabetes, it's important to understand the gut microbiome.
The gut microbiome is the collection of microorganisms that reside in the digestive tract. The microbiota has a significant impact on overall health, including glucose metabolism (Gurung et al., 2020).
The balance of microbiota in our gut can be influenced by many factors, including diet, lifestyle, and medication use (Chen et al., 2021). While some types of microbiota can be harmful to our health, others are beneficial and can help support healthy digestion and immune function.
If you thought your gut only played a role in producing some questionable sounds, think again! Believe it or not, gut health is strongly linked to diabetes, and taking care of it could help manage symptoms.
People with diabetes have a lower diversity of gut microbiota and studies have shown that different bacteria can be associated with insulin resistance or T2D (Chen et al., 2021). A higher abundance of butyrate-producing bacteria, are of particular interest because they produce a short-chain fatty acid called butyrate.
Butyrate plays a crucial role in maintaining gut health by reducing inflammation and supporting the intestinal barrier function. Several studies have shown that a higher abundance of butyrate-producing bacteria were associated with lower prevalence of T2D and insulin resistance (Qin et al., 2012; Hartstra et al., 2014).
Recent study further found out that people with T2D have lower microbial diversity in the gut, which may play a role in the development of T2D and may be linked to lower insulin sensitivity (Chen et al., 2021).
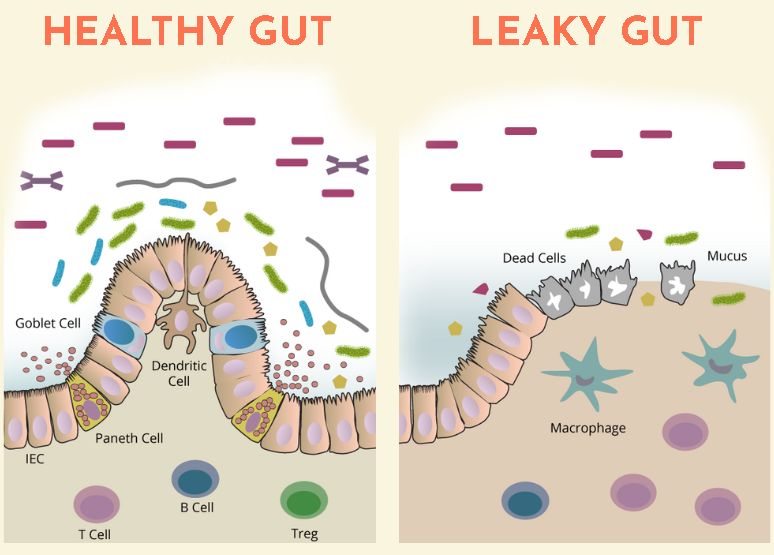
Intestinal permeability, also known as "leaky gut," is another issue that can arise from poor gut health. When the gut lining becomes compromised, toxins and bacteria can leak into the bloodstream, leading to inflammation and a host of health problems (Cani et al., 2007). T2D patients have significantly higher intestinal permeability than non-diabetics, allowing certain harmful substances like lipopolysaccharides (LPS, a toxin from bacteria) to enter the bloodstream (Horton et al., 2014). This may accelerate the development of insulin resistance and obesity further exacerbating the T2D symptoms (Sharma & Tripathi, 2019).
Taking antibiotics can change the mix of bacteria in the gut, which can be linked to the progression of diabetes.
For infants, using antibiotics a lot may lead to fewer types of bacteria in the gut and set the stage for diabetes by reducing beneficial bacteria like Bifidobacteria.
On the other hand, antibiotics may also offer some protection against T1D by promoting the growth of specific bacteria that encourage the development of protective immune cells in the gut. However, there’s still a lot we don’t understand about how changes in gut bacteria due to antibiotics might affect T1D, especially concerning the gut’s barrier function and inflammation (Sharma & Tripathi, 2019).
We know that specific bacteria present in the gut microbiota could control the sugar levels is in the blood (Hsieh et al., 2013). Supplementation with probiotics have been found to lower T2D indicators such as blood glucose, glycated haemoglobin, and c-peptide.
A more recent study showed that supplementation of probiotics reduced the total cholesterol, triglycerides, plasma glucose and insulin levels during fasting, which can support managing the implication of T2D (Kocsis et al., 2020).
Regular consumption of probiotic foods, such as kvass, yoghurt and kombucha, could be beneficial for either management or prevention of diabetes due to:

Changes in dietary patterns (calorie-dense, nutrient-deficient processed foods), sedentary lifestyles, and increased job demands are significant contributors to the onset and rapid progression of metabolic illnesses such as diabetes, atherosclerosis, and non-alcoholic fatty liver.
The development and treatment of metabolic disorders like T2D are greatly influenced by gut flora.
To regulate blood sugar levels and maintain healthy insulin sensitivity, it's important to maintain a balanced gut microbiota. This can be achieved through a healthy lifestyle, a balanced diet, and regular consumption of unprocessed, unpasteurised foods that contain live bacteria. Together, these strategies could serve as a highly effective therapeutic approach in managing not only T2D, but also other metabolic disorders.
Therefore, if you or a loved one has T2D, consider incorporating a raw, unpasteurised, unfiltered, and entirely plant-based live probiotic kvass into your diet.